Shopping Cart
CloseNo products in the cart.
Filter
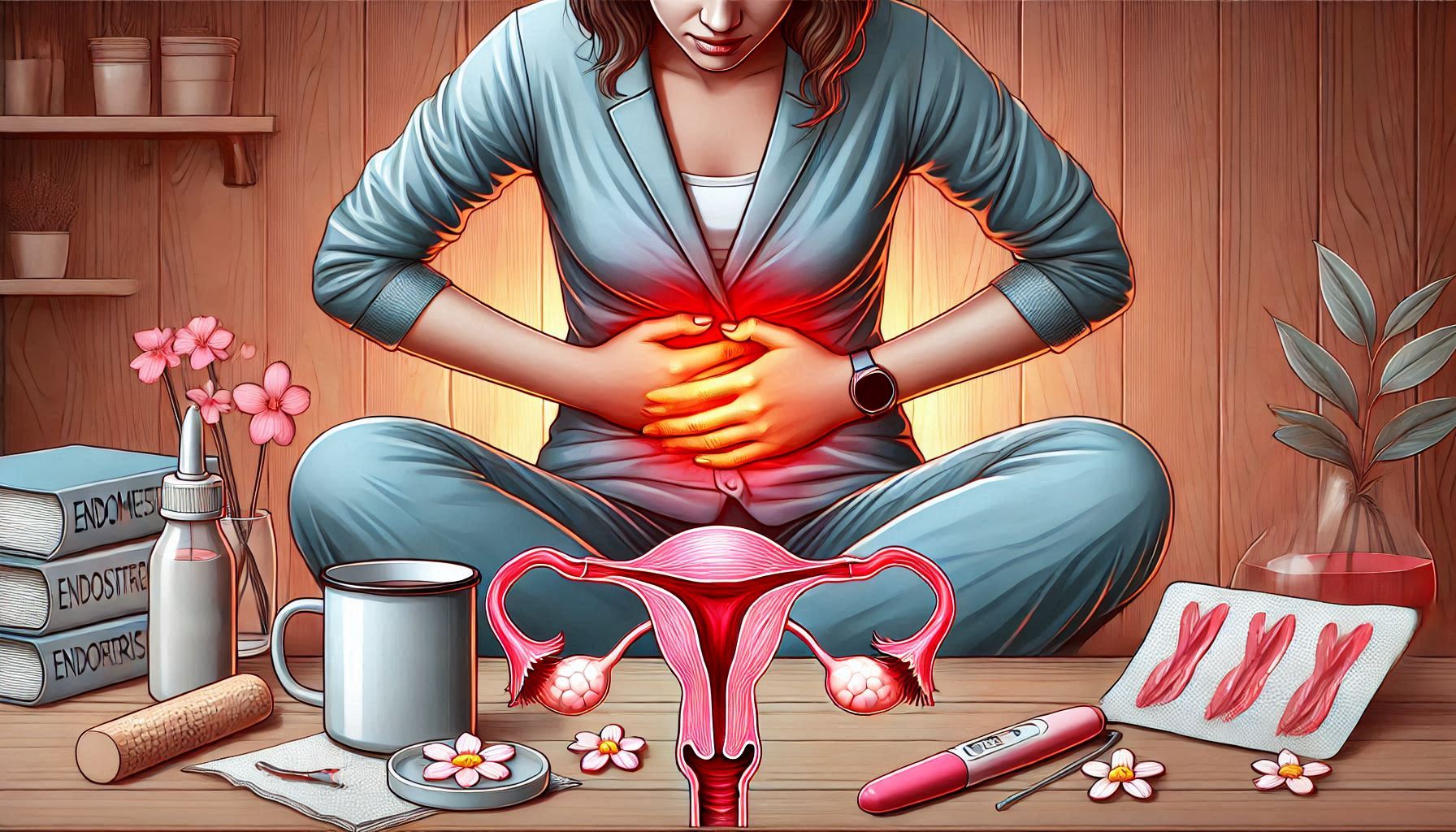
closeUnderstanding and Managing Endometriosis Pain: A Guide to Prevention and Relief
Author: ItHurts.com
A Comprehensive Talk on Understanding and Managing Endometriosis Pain
Understanding the Basics:
Endometriosis, a chronic condition affecting millions of women globally, is more than just a medical diagnosis—it’s a source of relentless, life-altering pain. Understanding the types of pain associated with endometriosis and how to address them is key to improving quality of life. In this guide, we’ll explore the intricacies of endometriosis pain, its causes, underlying reasons, and ways to manage and prevent it effectively.
Description of Pain: Types and Characteristics
Endometriosis pain manifests in various forms, each with unique characteristics and intensity:
Pelvic Pain
– Description: Persistent or intermittent ache in the lower abdomen or pelvis.
– Intensity: Ranges from mild discomfort to debilitating pain.
– Location: Often centered in the pelvis but may radiate to the lower back or thighs.
Dysmenorrhea (Painful Periods)
– Description: Severe cramps during menstruation, often more intense than typical menstrual discomfort.
– Intensity: Sharp, throbbing, or burning.
– Location: Primarily in the pelvic region but may extend to the back and legs.
Dyspareunia (Pain During Intercourse)
– Description: Pain during or after sexual activity, often deep and sharp.
– Intensity: Varies based on the depth and duration of intercourse.
– Location: Felt deep within the pelvis.
Gastrointestinal Pain
– Description: Abdominal pain resembling irritable bowel syndrome (IBS), often accompanied by bloating and constipation.
– Intensity: Can range from mild to severe.
– Location: Concentrated in the lower abdomen and pelvic area.
Nerve Pain
– Description: Sharp, shooting pains resulting from endometrial lesions pressing on nerves.
– Intensity: Severe and sudden.
– Location: Commonly in the pelvic region but may affect legs and lower back.
Causes of Pain
Endometriosis pain arises from several interconnected factors:
– Endometrial Lesions: Tissue similar to the uterine lining grows outside the uterus, causing inflammation and pain.
– Inflammation: Chronic inflammatory response around lesions amplifies discomfort.
– Scar Tissue (Adhesions): Abnormal scar tissue binds organs, leading to restricted movement and pain.
– Nerve Involvement: Lesions pressing on pelvic nerves can result in sharp, shooting pain.
– Hormonal Fluctuations: Hormonal changes during menstruation exacerbate pain symptoms.
Underlying Reasons for the Pain
The physiological and anatomical mechanisms behind endometriosis pain include:
Inflammatory Response
Endometrial-like tissue releases pro-inflammatory chemicals, leading to localized swelling and pain. Cytokines and prostaglandins amplify the body’s pain signals.
Nerve Compression
Lesions near pelvic nerves can cause nerve compression, resulting in pain that radiates to the lower back, legs, or groin.
Organ Dysfunction
Scar tissue can tether organs like the bladder or bowels, causing pain during urination or bowel movements.
Hormonal Sensitivity
The misplaced endometrial tissue responds to menstrual cycle hormones, leading to cyclical pain and cramping.
Presentation of the Pain
Endometriosis pain often follows a predictable pattern but can vary widely between individuals. It may:
– Worsen during menstruation or ovulation.
– Occur sporadically or as a chronic, daily pain.
– Flare up after physical activity, sexual intercourse, or stress.
– Accompany symptoms like fatigue, nausea, or heavy menstrual bleeding.
Treatment and Relief for Existing Pain
Managing endometriosis pain requires a multifaceted approach. Here are actionable strategies:
Lifestyle Adjustments
– Dietary Changes:
– Incorporate anti-inflammatory foods like fatty fish, leafy greens, and nuts.
– Reduce red meat and processed foods, which may trigger inflammation.
– Heat Therapy:
– Use heating pads or warm baths to relax muscles and reduce pain.
Exercises and Stretches
– Yoga Poses:
– Child’s Pose (Balasana): Eases pelvic tension.
– Cat-Cow Stretch: Alleviates lower back pain.
– Pelvic Floor Exercises:
– Strengthen muscles to reduce dyspareunia.
Self-Massage Techniques
– Use gentle abdominal massage to improve blood flow and reduce inflammation:
– Massage in circular motions using warm oils like lavender or chamomile.
Holistic Approaches
– Acupuncture: Targets pain points and reduces inflammation.
– Aromatherapy: Essential oils like clary sage and lavender can help relieve stress and pain.
Medical Treatments
– Medication:
– Non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief.
– Hormonal therapies (e.g., birth control pills) to suppress endometrial tissue growth.
– Surgical Options:
– Laparoscopy to remove endometrial lesions and scar tissue.
Scientific Research on Endometriosis Pain
Research underscores the complexity of endometriosis pain. A 2020 study in *The Lancet* highlighted that endometriosis affects up to 10% of women of reproductive age and is often underdiagnosed due to its diverse symptom presentation. Another study published in *Human Reproduction Update* noted that hormonal treatments, combined with lifestyle modifications, show significant promise in managing symptoms.
Emerging therapies like neuromodulation and gene-based treatments are currently being explored to target pain at its source more effectively.
Scientific Research on Endometriosis Pain
While endometriosis cannot be cured, proactive steps can minimize its impact:
Maintain Hormonal Balance
– Use hormonal contraceptives under medical supervision to regulate cycles.
Adopt Anti-Inflammatory Habits
– Follow a Mediterranean diet rich in omega-3s and antioxidants.
– Stay hydrated and avoid inflammatory triggers like caffeine and alcohol.
Practice Stress Management
– Use relaxation techniques like meditation, deep breathing, or mindfulness to lower stress levels, which can exacerbate pain.
Ergonomic Posture
– Invest in ergonomic seating and maintain good posture to reduce pelvic strain.
Regular Physical Activity
– Engage in low-impact exercises like swimming or pilates to improve circulation and reduce adhesions.
Final Thoughts:
Endometriosis pain is multifaceted, affecting physical, emotional, and social well-being. Understanding its types, causes, and underlying mechanisms empowers individuals to take control of their symptoms. From dietary changes and holistic therapies to advanced medical interventions, various strategies exist to manage and prevent pain.
Take Action
If you or someone you know struggles with endometriosis pain, start by consulting a healthcare professional for a personalized management plan. Small lifestyle changes and informed decisions can significantly improve quality of life. Prioritize your health—relief and a better life are within reach.
ItHurts.com is your ally in your endeavor to live pain-free. We offer guidance, resources, and community support to address chronic pain, emotional stress, and physical discomfort. Discover insightful articles, product reviews, recommendations and shared experiences to empower your journey to better health. Remember, if it hurts, we can help!
Related Products
No posts found!
Related Blogs
No posts found!
