They usually show up on your fingers, toes, nose, and ears—the extremities you probably forgot to cover with enough layers. They’re mostly harmless and will eventually go away when the weather gets warm (lucky you!), but in the meantime, they’ll be a burning, itching, painful reminder that you are, in fact, sensitive to the cold. Don’t scratch them, unless you’re aiming for a secondary infection—because who doesn’t love a two-for-one medical crisis? Pro-Tip: Warm up slowly. Think of your cold skin as a delicate flower, not a frozen pizza you need to blast in the microwave.
Inflammation, Recovery & Longevity: Why Function Health Testing Is Becoming So Popular Inflammation is at the root of fatigue, soreness, slow recovery, brain fog, and long-term conditions. Yet most people never get inflammation markers checked beyond the basics. Function Health includes multiple inflammation-related biomarkers inside their testing panel — giving you a deep look into the way your body is healing or struggling. ⭐ Why Inflammation Matters Low-grade inflammation can affect: 🔥 Muscle recovery🔥 Energy levels🔥 Metabolism🔥 Sleep quality🔥 Hormone balance🔥 Longevity Most people think inflammation is only related to injury — but internal inflammation can be silent for years. ⭐ Biomarkers Related to Inflammation & Recovery Function testing may include markers for: Inflammation levels Oxidative stress Liver & kidney detox pathways Nutrient levels affecting recovery Hormone signals involved in stress & repair Blood sugar and metabolic strain These markers help explain why you may feel “off” even when basic bloodwork looks normal. ⭐ Real Stories: How People Found Clarity Insert these video reviews: “These 7 Lab Tests Can Help You Manage Your Weight” “4 Ways Inflammation Hinders Muscle-Building” “These Advanced Lab Tests Can Reveal Why You’re Always Hungry” Each one gives clear, simple explanations that your readers will connect with. ⭐ For Athletes & Regular People Alike Whether you’re training intensely or simply trying to feel better: Tracking inflammation Seeing nutrient deficiencies Understanding metabolism Monitoring hormone shifts …can make a dramatic difference. Function Health makes this accessible in one simple test. ⭐ Your Path to Better Recovery Starts With Knowledge Understanding your internal markers helps you: ✔ Train smarter✔ Recover faster✔ Prevent burnout✔ Improve longevity✔ Manage fatigue & soreness ⭐ Start Your Function Health Test Start Function Health Testing
Hormones, Mood & Metabolism: What Your Biomarkers Say About You (And Why Function Health Makes It Easy) Hormones control almost everything — energy, mood, hunger, weight, sleep.But most people never get a full hormone panel unless they’re already very sick. Function Health changes that by including complete hormone testing inside their 100+ biomarker panel. You get a full picture, not just one or two numbers. ⭐ What Hormones Are Tested? Function Health may include markers that relate to: Thyroid function (important for metabolism & mood) Cortisol (stress response) Key sex hormones Hormone-related metabolism markers Many people don’t realize how dramatically hormones influence everyday life: ✔ Feeling “wired but tired”✔ Crashing after meals✔ Unexplained anxiety✔ Mood swings✔ Weight fluctuations✔ Poor sleep These are often connected to biomarkers — and Function Health helps you see the patterns. ⭐ Why This Matters for Women & Men Women often go years without proper hormone evaluation.Men often ignore hormone imbalance until symptoms become severe. Function Health lets you see your numbers in a simple dashboard without needing a specialist appointment first . ⭐ Real Member Stories (Add Video Thumbnails) Emeline’s Story – Understanding the hormone imbalances that shaped her mood Chelsea’s Story – Finding clarity after years of unexplained symptoms Danielle’s Story – Identifying inflammation & hormonal trends ⭐ How the Dashboard Helps You Understand Your Body The insights include: Whether a biomarker is optimal What it means for your body Why levels may be high or low What actions might help How your results compare over time This is the “missing piece” in traditional healthcare. ⭐ Your Health, But Clearer Function Health doesn’t diagnose — it enlightens.It helps you see the bigger picture so you can: Talk to your doctor with confidence Track progress Prevent issues before they become serious Understand what your body is trying to tell you ⭐ Start Your Hormone + Full Body Testing Start Function Health Testing
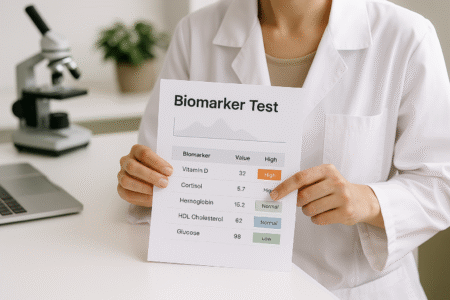
Why 100+ Biomarkers Matter: How Function Health Helps You Understand Your Whole Body Have you ever been told your bloodwork is “normal,” yet you still feel exhausted, foggy, or inflamed? This is one of the biggest gaps in traditional healthcare — and exactly where Function Health steps in. Traditional labs usually check 8–12 basic markers . Function Health checks 100+ clinician-reviewed biomarkers spanning hormones, inflammation, metabolism, liver, kidneys, thyroid, nutrients, cholesterol, and longevity markers. The goal?To help you understand the “why” behind your symptoms, not just get a number. ⭐ What Function Health Measures (and Why It Matters) Your body works like a network — hormones influence mood, inflammation affects sleep, nutrient levels shape energy. Function Health labs look at over 100 biomarkers across: Hormones (thyroid, cortisol, sex hormones) Metabolism & weight regulation Liver & kidney health Inflammation levels Vitamin & mineral deficiencies Blood sugar & insulin resistance Heart health markers Long-term health & aging markers For many people, this becomes the first time they receive a complete health picture instead of isolated lab numbers. ⭐ A Simple Process With Deep Insight Join Function Health (affiliate link here) Get your lab order within minutes Visit a nearby partnered lab Receive your results in your dashboard View your biomarkers with easy explanations Every marker includes a clear explanation, ranges, color-coded insights, and helpful guidance. ⭐ Why Members Love It (Real Stories) Insert these videos to increase engagement: Aimee’s Story (1:00) Guhan’s Story (0:47) Rebecca’s Story (2:09) Patients consistently praise how Function Health helped them: 🌱 Understand hormones⚡ Improve energy🧠 Decode brain fog🔥 Identify inflammation🩺 Track trends over time ⭐ Is Function Health Right for You? Function Health is ideal if you want to: Understand why you feel tired Track metabolic or hormonal changes Focus on prevention Get clear insights without rushing doctor visits Take control of your health data If you’ve ever thought, “I know something’s off, but nobody can explain it,” — these labs can help provide clarity. ⭐ Start Your Deep Health Testing Ready to uncover the biomarkers behind your symptoms? Start Function Health Testing
Clear Skin, Clear Mind: How Sesame Helps You Treat Acne, Rashes, Hair Loss & More From Home Skin problems affect more than appearance — they affect confidence, mood, and daily comfort. Acne, rashes, eczema, rosacea, or sudden hair loss can feel overwhelming, especially when you can’t get a quick appointment with a dermatologist. Many people wait months to see a specialist, struggle with expensive treatments, or feel embarrassed discussing their symptoms in person.But now, telehealth makes expert skin care more accessible. Sesame Care connects you directly with licensed dermatology clinicians who can diagnose issues, prescribe treatments, and guide you through a personalized skincare plan — all online and without insurance. ⭐ Skin & Hair Issues Sesame Dermatology Can Treat Mild to severe acne Hormonal acne Eczema flare-ups Psoriasis Rosacea Rashes and skin irritation Dark spots & hyperpigmentation Scalp conditions Dandruff Hair thinning or early hair loss Prescription skincare These concerns are extremely common — and treatable with the right guidance. 💬 Why Getting Skin Help Is Often Difficult Most people with skin issues experience: “Long waiting times for appointments.”“Very high dermatology costs.”“Confusion choosing over-the-counter products.”“Embarrassment discussing symptoms in person.”“No clear plan or follow-up.” Telehealth solves many of these problems by offering easier and faster access. 🖥️ Why Sesame Works Well for Skin Care With Sesame, you can: Book licensed dermatology clinicians online Get same-day or next-day appointments Share photos of your skin Receive diagnosis & personalized treatment Get prescription creams, gels, or oral medications Have meds delivered (in eligible states) Follow up at low cost Everything is simple, private, and handled from home. 🧴 Common Diagnoses & Treatments on Sesame Acne Providers may prescribe: Retinoids Benzoyl peroxide combinations Topical antibiotics Oral medications (if necessary) Hormonal acne support Eczema & Rashes Treatment can include: Anti-inflammatory creams Anti-itch medications Triggers & lifestyle guidance Hair Loss Clinicians may recommend: Minoxidil Finasteride Nutrient testing Scalp treatment plans Rosacea Controlled with: Anti-inflammatory creams Prescription gels Redness reduction strategies You get a real treatment plan — not random skincare guessing. 📊 Dermatology Clinic vs Sesame In-Person Dermatology Sesame Dermatology Long wait lists Same-day availability Expensive visits Affordable upfront pricing Requires insurance No insurance needed Embarrassing conversations Private online consult Limited scheduling Choose any time slot Sesame is especially helpful for those who want fast, judgment-free care. 💡 Why Skin Issues Affect Your Mental Health Skin concerns can cause: Low confidence Anxiety in social situations Stress about appearance Frustration from trying multiple products Avoidance of mirrors or photos Treating the skin often improves overall emotional wellbeing too. 🩺 What Happens During a Sesame Dermatology Visit? A typical consult includes: A review of your concerns Photo upload of affected skin areas Questions about your routine & triggers Diagnosis Treatment plan Prescription (if medically appropriate) Follow-up recommendations It’s quick, comfortable, and tailored to you. ✔️ Why People Love Sesame for Skin Care Straightforward pricing Licensed clinicians No waiting months Fast prescriptions Personalized plans Convenient follow-ups Great for teens, adults, and hormones-related skin concerns 🖤 Ready to Treat Your Skin From Home? You can book an affordable Dermatology visit on Sesame — no insurance required. Book a Skin or Hair Visit
Women’s Health Made Simple: How Sesame Helps With Hormones, PCOS, UTIs & More Women deal with a wide range of health issues that often go untreated because of long wait times, discomfort discussing symptoms, or doctors dismissing concerns as “normal.” But many of these problems have real underlying causes — and they deserve proper care. Hormonal changes, infections, cycle irregularities, PMS, PCOS, and menopause symptoms can all impact your daily life. And when these issues are ignored, they affect your energy, mood, productivity, confidence, and overall wellbeing. Sesame Care makes it easier for women to get fast, affordable help from licensed clinicians — without insurance, referrals, or months-long delays. ⭐ Common Women’s Health Issues Sesame Treats Irregular periods PMS / PMDD PCOS symptoms Yeast infections UTIs (urinary tract infections) Vaginal discomfort Birth control consults Acne & hormonal skin issues Low libido or mood changes Menopause-related symptoms These concerns are common — and treatable. 💬 Why Women Often Struggle to Get Answers Many women report experiences such as: “My doctor said it’s normal.”“I waited months for an appointment.”“They ran no tests.”“They told me to just take painkillers.”“I felt rushed and unheard.” Telehealth is changing that by making it easier to access clinicians who take women’s symptoms seriously. 🖥️ How Sesame Supports Women’s Health Sesame offers direct access to licensed women’s health clinicians who can help with: Online diagnosis & treatment Prescription medication (when appropriate) Birth control options PCOS support Cycle regulation help UTI & yeast infection treatment Menopause care & symptom relief No waiting rooms. No insurance paperwork.Just simple, private care from home. 🧬 Conditions Often Linked to Hormones A Sesame clinician may look deeper if you experience: Sudden weight gain Hair loss Irregular cycles Acne breakouts Mood swings Low energy Sleep problems Hot flashes Brain fog Many of these symptoms connect to estrogen, progesterone, testosterone, or thyroid imbalances. 📊 Quick Comparison: Traditional Gynecology vs Sesame Traditional Women’s Health Sesame Care Long wait times Same-day visits Requires insurance No insurance needed Sensitive symptoms feel awkward Private, comfortable online visit Limited appointment availability Wide provider choice Surprise bills Clear upfront pricing 🌼 Fast Relief for Common Problems UTIs Treatment usually includes a quick virtual review and a prescription sent to your pharmacy the same day. Yeast Infections Doctors can diagnose symptoms online and prescribe antifungals when appropriate. PCOS & Hormonal Issues Clinicians help manage symptoms like irregular periods, acne, fatigue, and insulin resistance. Birth Control Consults You can discuss options and get a prescription without an in-person visit. 🩺 What to Expect During a Sesame Visit A typical women’s health visit includes: Discussion of symptoms Questions about your cycle & medical history Possible lab recommendations Diagnosis or next steps Prescription (if medically appropriate) Follow-up plan The process is calm, private, and supportive. 💬 Why Women Love Sesame Appointments start as low as $25–$45 Same-day availability Licensed clinicians Zero insurance barriers Private + judgment-free Clear, upfront pricing Women repeatedly say they finally feel heard, respected, and understood . 🖤 Ready to Get Help Today? You can book a Women’s Health visit on Sesame anytime — with no insurance required. Book a Women’s Health Visit