Beyond the Blues: Preventing and Reducing Depression-Related Pain Author: ItHurts.com A Comprehensive Talk on Depression and Chronic Pain Understanding the Basics: When discussing depression, the focus often revolves around emotional well-being, yet its physical manifestations—commonly referred to as depression-related pain—are just as impactful. This pain, which includes headaches, muscle aches, and deep fatigue, often compounds the challenges of mental health struggles. Fortunately, understanding, treating, and preventing this pain is possible with a combination of awareness, proactive care, and evidence-based strategies. Description of Depression-Related Pain Depression-related pain manifests in several forms, often varying from person to person: – Headaches: These are tension-type headaches characterized by a dull, constant ache, typically felt around the forehead or temples. Unlike migraines, they do not involve nausea or sensitivity to light. – Muscle Aches and Joint Pain: Generalized muscle stiffness, soreness, and joint discomfort are common. The pain can feel similar to fibromyalgia, a condition marked by widespread musculoskeletal pain. – Chest Pain: Depression can intensify the perception of chest pain, often mistaken for heart issues. It may stem from increased tension in the chest muscles or the physiological effects of stress. – Back Pain: Persistent back pain often accompanies depression, exacerbated by poor posture, inactivity, or stress-related muscle tension. – Fatigue and Body Aches: A profound sense of physical exhaustion, coupled with aching muscles and joints, is a hallmark of depression-related pain. Underlying Reasons for Depression-Related Pain Physiological and anatomical reasons behind depression-related pain include: – Neurotransmitter Imbalance: Low levels of serotonin and norepinephrine reduce the body’s ability to suppress pain signals. – Cortisol Dysregulation: Prolonged stress and depression elevate cortisol levels, leading to chronic inflammation and heightened pain sensitivity. – Autonomic Nervous System Dysfunction: Depression can alter the balance between the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) systems, resulting in persistent muscle tension and nerve irritation. – Central Sensitization: In some cases, depression causes the central nervous system to amplify pain signals, a phenomenon seen in conditions like fibromyalgia. Causes of Depression-Related Pain Several factors contribute to depression-related pain: – Psychological Stress: Chronic stress associated with depression triggers muscle tension and inflammation. – Altered Brain Chemistry: Changes in neurotransmitters like serotonin and dopamine impact the brain’s ability to regulate pain perception. – Sleep Disturbances: Depression often leads to insomnia or disrupted sleep, which impairs the body’s ability to repair itself, increasing sensitivity to pain. – Reduced Physical Activity: Depression discourages movement, leading to stiffness and muscle weakness. – Comorbid Conditions: Conditions like anxiety, fibromyalgia, or irritable bowel syndrome (IBS) often coexist with depression, amplifying pain. Presentation of Depression-Related Pain Depression-related pain often presents itself in a subtle yet persistent manner: – The pain is diffuse and difficult to localize. – It is often described as a “heaviness” or “aching” sensation. – Symptoms may worsen during periods of heightened stress or sadness. – Pain is often accompanied by fatigue, lethargy, and a sense of physical heaviness. This pain can be confusing for those experiencing it, as there may be no obvious physical cause, which can lead to feelings of frustration or hopelessness. Treatment and Relief for Existing Pain While depression-related pain can feel overwhelming, various strategies provide effective relief: Physical Exercises and Stretches – Engage in low-impact aerobic exercises such as walking, swimming, or yoga to release endorphins. – Perform stretches targeting tension-prone areas like the neck, shoulders, and back. – Strength training can improve muscle tone and reduce stiffness. Self-Massage Techniques – Use foam rollers to release muscle knots and improve circulation. – Massage tense areas using essential oils like lavender or eucalyptus for added relaxation. – Apply heat pads or warm baths to loosen tight muscles. Holistic Approaches – Mindfulness Meditation: Focused breathing and mindfulness techniques can reduce perceived pain intensity. – Acupuncture: Studies show that acupuncture helps reduce pain by promoting natural painkillers in the body, such as endorphins. – Aromatherapy: Lavender oil has been shown to reduce stress and muscle tension when used in a diffuser or bath. Medical Treatments – Antidepressants: Medications like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) help regulate pain perception. – Physical Therapy: Tailored therapy can address specific muscle imbalances and improve posture. – Pain Management Clinics: These provide a multidisciplinary approach to chronic pain management. Actionable Steps for Preventing Depression-Related Pain Proactive measures can significantly reduce the risk of depression-related pain: 1. Maintain Good Posture – Use ergonomic chairs that support the natural curvature of the spine. – Position screens at eye level to avoid neck strain. – Take breaks to stretch during prolonged sitting. 2. Create a Regular Exercise Routine – Incorporate at least 150 minutes of moderate exercise weekly. – Focus on activities you enjoy to ensure consistency. 3. Stress Management – Practice mindfulness meditation or yoga daily. – Engage in hobbies or activities that bring joy and relaxation. – Seek therapy or counseling for chronic stress management. 4. Prioritize Sleep Hygiene – Maintain a consistent sleep schedule. – Limit screen time before bed. – Create a calming bedtime routine, such as reading or listening to relaxing music. 5. Balanced Nutrition – Consume foods rich in omega-3 fatty acids, magnesium, and vitamin D, all linked to improved mood and pain regulation. – Stay hydrated to reduce muscle cramps and fatigue. Final Thoughts: Depression-related pain is a complex and multifaceted challenge, but with the right knowledge and tools, it can be effectively managed and even prevented. By understanding its causes, addressing underlying physiological factors, and adopting proactive strategies, individuals can alleviate pain and improve their quality of life. Remember, no one needs to face this journey alone. Consult healthcare professionals for tailored treatments, and consider joining support groups or communities for encouragement and shared experiences. Take the first step today toward a healthier, pain-free tomorrow. Your body—and mind—will thank you. ItHurts.com is your ally in your endeavor to live pain-free. We offer guidance, resources, and community support to address chronic pain, emotional stress, and physical discomfort. Discover insightful articles, product reviews, recommendations and shared experiences to
Understanding Fibromyalgia Pain: Prevention and Relief Strategies Author: ItHurts.com A Comprehensive Talk on Fibromyalgia Understanding the Basics: Fibromyalgia is a complex, chronic condition characterized by widespread pain, fatigue, and a host of other symptoms. For individuals living with this condition, managing pain can feel overwhelming. However, with the right knowledge and strategies, it’s possible to reduce the intensity of symptoms and prevent flare-ups. This comprehensive guide delves into the characteristics, causes, underlying reasons, presentation, treatment options, scientific insights, and actionable steps for preventing fibromyalgia pain. Description of Fibromyalgia Pain Fibromyalgia pain manifests in various ways, often leaving individuals feeling like their entire body is affected. Here are the common characteristics: – Widespread Muscular Pain: A persistent, deep ache felt across the body, often in muscles and connective tissues. – Tender Points: Specific areas, such as the neck, shoulders, hips, and knees, are highly sensitive to pressure. – Neuropathic Pain: A burning, tingling, or shooting pain, often described as pins-and-needles sensations. – Fatigue-Related Pain: Exacerbated by lack of restorative sleep, leading to heightened muscle soreness and stiffness. – Allodynia: Pain triggered by stimuli that wouldn’t normally be painful, such as light touches or clothing pressure. Intensity and Location The intensity of fibromyalgia pain varies. Some individuals experience mild discomfort, while others endure debilitating pain that impacts daily activities. Locations of pain often include the back, shoulders, neck, hips, and knees, but it can spread to virtually any part of the body. Causes of Fibromyalgia Pain The exact cause of fibromyalgia remains unclear, but research points to several potential triggers: – Central Sensitization: An increased sensitivity in the brain and spinal cord to pain signals. – Trauma or Injury: Physical trauma, such as car accidents or sports injuries, may act as a trigger. – Emotional Stress: Chronic stress and anxiety are linked to the onset and exacerbation of fibromyalgia. – Genetics: A family history of fibromyalgia increases the likelihood of developing the condition. – Infections: Certain illnesses, such as Epstein-Barr virus, may contribute to its development. Underlying Reasons for Fibromyalgia Pain Fibromyalgia pain stems from complex physiological and neurological mechanisms. Some key contributors include: – Hyperactive Nerve Responses: Overactive nerve endings amplify pain signals sent to the brain. – Muscle Dysfunction: Persistent tension and microtears in muscles may lead to stiffness and soreness. – Imbalanced Neurotransmitters: Low serotonin and dopamine levels can reduce pain tolerance. – Hypersensitivity of Pain Pathways: Central sensitization causes heightened responses to pain stimuli. – Autonomic Nervous System Dysregulation: Disruptions in the autonomic nervous system contribute to fatigue and muscle pain. Presentation of Fibromyalgia Pain Fibromyalgia pain often appears alongside other symptoms, which can make it difficult to diagnose: – Morning Stiffness: Many individuals feel most pain upon waking, with muscles and joints feeling stiff. – Migrating Pain: Pain often moves from one area to another without clear explanation. – Pain Flare-Ups: Stress, weather changes, or overexertion can trigger episodes of heightened pain. – Fatigue and Cognitive Issues: Pain is often accompanied by “fibro fog,” or difficulty concentrating. Treatment and Relief for Existing Pain Relieving fibromyalgia pain involves a combination of lifestyle adjustments, holistic approaches, and medical interventions: Lifestyle Strategies – Regular Exercise: Low-impact activities like swimming, yoga, and tai chi help improve muscle flexibility and reduce pain. – Sleep Hygiene: Maintain consistent sleep schedules and optimize the sleep environment to improve rest. – Stress Management: Incorporate relaxation techniques, such as meditation and deep breathing. Self-Care Techniques – Gentle Stretches: Focus on lengthening tight muscles with slow, deliberate movements. – Self-Massage: Use a foam roller or massage tools to release muscle knots. – Warm Baths: Soaking in Epsom salt baths can reduce soreness. Holistic Therapies – Acupuncture: May help relieve muscle pain and improve energy flow. – Aromatherapy: Essential oils, such as lavender, can promote relaxation. – Dietary Adjustments: Anti-inflammatory diets rich in omega-3 fatty acids and whole foods may help. Medical Interventions – Medications: Options include pain relievers, antidepressants (like amitriptyline), and anticonvulsants (such as pregabalin). – Physical Therapy: Tailored exercise plans can strengthen muscles and improve posture. – Trigger Point Injections: Targeted injections provide relief for tender points. Scientific Research on Fibromyalgia Pain Scientific studies provide valuable insights into fibromyalgia: – A 2020 study in *Arthritis Research & Therapy* highlighted the role of central sensitization in amplifying pain signals. – Research from the *Journal of Pain Research* (2022) found that mindfulness-based stress reduction significantly improves fibromyalgia symptoms. – A systematic review in *The Clinical Journal of Pain* confirmed that aerobic and resistance training effectively reduce pain severity. Actionable Steps for Preventing Fibromyalgia Pain While fibromyalgia cannot be cured, there are proactive steps you can take to minimize flare-ups: Physical Wellness Exercise Regularly: Engage in moderate, low-impact activities for 20–30 minutes, 3–5 times a week. Improve Posture: Use ergonomic furniture and be mindful of posture when sitting or standing. Stretch Daily: Incorporate stretches that target common areas of stiffness. Stress Management Practice Relaxation: Dedicate time to activities that reduce stress, such as journaling or yoga. Establish Boundaries: Limit activities that cause physical or emotional strain. Diet and Nutrition Stay Hydrated: Drink plenty of water to support muscle function. Choose Anti-Inflammatory Foods: Focus on fruits, vegetables, whole grains, and lean proteins. Avoid Triggers: Identify and limit foods that exacerbate symptoms, such as caffeine and processed foods. Sleep Hygiene Create a Relaxing Routine: Unwind before bed with calming activities. Optimize the Bedroom: Use blackout curtains and keep the room cool and quiet. Avoid Stimulants: Limit caffeine and screen time before sleep. Final Thoughts: Fibromyalgia pain is multifaceted, stemming from both physical and neurological factors. While the condition can be challenging, individuals can take steps to manage and prevent symptoms effectively. By incorporating regular exercise, practicing stress management, and pursuing holistic and medical treatments, individuals can significantly improve their quality of life. Key Takeaways: – Understand your pain and triggers to create personalized strategies. – Adopt a proactive approach with consistent physical activity, proper nutrition, and stress reduction. – Seek support from healthcare professionals and fibromyalgia communities. Living with
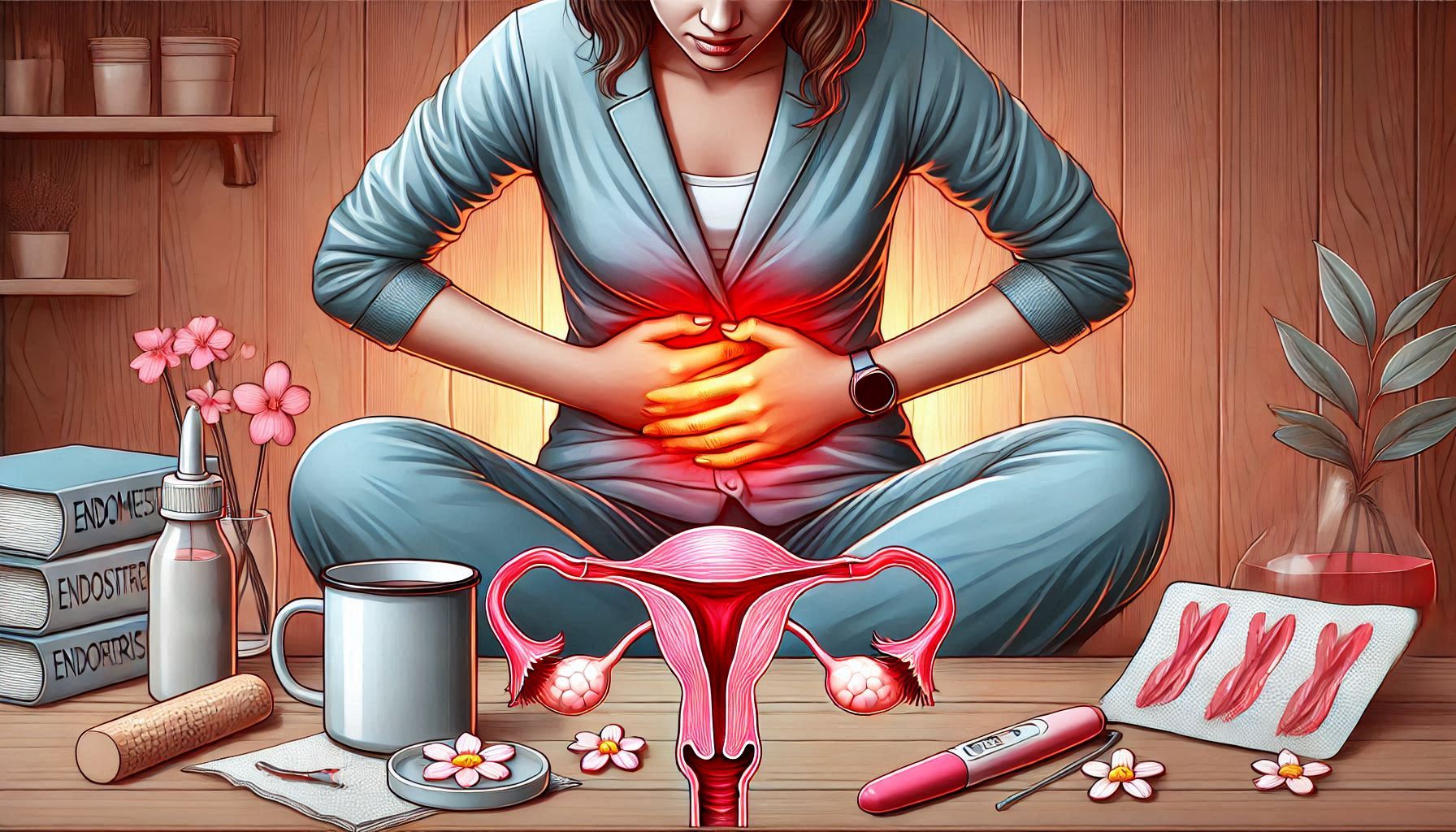
Understanding and Managing Endometriosis Pain: A Guide to Prevention and Relief Author: ItHurts.com A Comprehensive Talk on Understanding and Managing Endometriosis Pain Understanding the Basics: Endometriosis, a chronic condition affecting millions of women globally, is more than just a medical diagnosis—it’s a source of relentless, life-altering pain. Understanding the types of pain associated with endometriosis and how to address them is key to improving quality of life. In this guide, we’ll explore the intricacies of endometriosis pain, its causes, underlying reasons, and ways to manage and prevent it effectively. Description of Pain: Types and Characteristics Endometriosis pain manifests in various forms, each with unique characteristics and intensity: Pelvic Pain – Description: Persistent or intermittent ache in the lower abdomen or pelvis. – Intensity: Ranges from mild discomfort to debilitating pain. – Location: Often centered in the pelvis but may radiate to the lower back or thighs. Dysmenorrhea (Painful Periods) – Description: Severe cramps during menstruation, often more intense than typical menstrual discomfort. – Intensity: Sharp, throbbing, or burning. – Location: Primarily in the pelvic region but may extend to the back and legs. Dyspareunia (Pain During Intercourse) – Description: Pain during or after sexual activity, often deep and sharp. – Intensity: Varies based on the depth and duration of intercourse. – Location: Felt deep within the pelvis. Gastrointestinal Pain – Description: Abdominal pain resembling irritable bowel syndrome (IBS), often accompanied by bloating and constipation. – Intensity: Can range from mild to severe. – Location: Concentrated in the lower abdomen and pelvic area. Nerve Pain – Description: Sharp, shooting pains resulting from endometrial lesions pressing on nerves. – Intensity: Severe and sudden. – Location: Commonly in the pelvic region but may affect legs and lower back. Causes of Pain Endometriosis pain arises from several interconnected factors: – Endometrial Lesions: Tissue similar to the uterine lining grows outside the uterus, causing inflammation and pain. – Inflammation: Chronic inflammatory response around lesions amplifies discomfort. – Scar Tissue (Adhesions): Abnormal scar tissue binds organs, leading to restricted movement and pain. – Nerve Involvement: Lesions pressing on pelvic nerves can result in sharp, shooting pain. – Hormonal Fluctuations: Hormonal changes during menstruation exacerbate pain symptoms. Underlying Reasons for the Pain The physiological and anatomical mechanisms behind endometriosis pain include: Inflammatory Response Endometrial-like tissue releases pro-inflammatory chemicals, leading to localized swelling and pain. Cytokines and prostaglandins amplify the body’s pain signals. Nerve Compression Lesions near pelvic nerves can cause nerve compression, resulting in pain that radiates to the lower back, legs, or groin. Organ Dysfunction Scar tissue can tether organs like the bladder or bowels, causing pain during urination or bowel movements. Hormonal Sensitivity The misplaced endometrial tissue responds to menstrual cycle hormones, leading to cyclical pain and cramping. Presentation of the Pain Endometriosis pain often follows a predictable pattern but can vary widely between individuals. It may: – Worsen during menstruation or ovulation. – Occur sporadically or as a chronic, daily pain. – Flare up after physical activity, sexual intercourse, or stress. – Accompany symptoms like fatigue, nausea, or heavy menstrual bleeding. Treatment and Relief for Existing Pain Managing endometriosis pain requires a multifaceted approach. Here are actionable strategies: Lifestyle Adjustments – Dietary Changes: – Incorporate anti-inflammatory foods like fatty fish, leafy greens, and nuts. – Reduce red meat and processed foods, which may trigger inflammation. – Heat Therapy: – Use heating pads or warm baths to relax muscles and reduce pain. Exercises and Stretches – Yoga Poses: – Child’s Pose (Balasana): Eases pelvic tension. – Cat-Cow Stretch: Alleviates lower back pain. – Pelvic Floor Exercises: – Strengthen muscles to reduce dyspareunia. Self-Massage Techniques – Use gentle abdominal massage to improve blood flow and reduce inflammation: – Massage in circular motions using warm oils like lavender or chamomile. Holistic Approaches – Acupuncture: Targets pain points and reduces inflammation. – Aromatherapy: Essential oils like clary sage and lavender can help relieve stress and pain. Medical Treatments – Medication: – Non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief. – Hormonal therapies (e.g., birth control pills) to suppress endometrial tissue growth. – Surgical Options: – Laparoscopy to remove endometrial lesions and scar tissue. Scientific Research on Endometriosis Pain Research underscores the complexity of endometriosis pain. A 2020 study in *The Lancet* highlighted that endometriosis affects up to 10% of women of reproductive age and is often underdiagnosed due to its diverse symptom presentation. Another study published in *Human Reproduction Update* noted that hormonal treatments, combined with lifestyle modifications, show significant promise in managing symptoms. Emerging therapies like neuromodulation and gene-based treatments are currently being explored to target pain at its source more effectively. Scientific Research on Endometriosis Pain While endometriosis cannot be cured, proactive steps can minimize its impact: Maintain Hormonal Balance – Use hormonal contraceptives under medical supervision to regulate cycles. Adopt Anti-Inflammatory Habits – Follow a Mediterranean diet rich in omega-3s and antioxidants. – Stay hydrated and avoid inflammatory triggers like caffeine and alcohol. Practice Stress Management – Use relaxation techniques like meditation, deep breathing, or mindfulness to lower stress levels, which can exacerbate pain. Ergonomic Posture – Invest in ergonomic seating and maintain good posture to reduce pelvic strain. Regular Physical Activity – Engage in low-impact exercises like swimming or pilates to improve circulation and reduce adhesions. Final Thoughts: Endometriosis pain is multifaceted, affecting physical, emotional, and social well-being. Understanding its types, causes, and underlying mechanisms empowers individuals to take control of their symptoms. From dietary changes and holistic therapies to advanced medical interventions, various strategies exist to manage and prevent pain. Take Action If you or someone you know struggles with endometriosis pain, start by consulting a healthcare professional for a personalized management plan. Small lifestyle changes and informed decisions can significantly improve quality of life. Prioritize your health—relief and a better life are within reach. ItHurts.com is your ally in your endeavor to live pain-free. We offer guidance, resources, and community support to address chronic pain, emotional stress, and physical discomfort. Discover insightful articles, product reviews, recommendations and shared experiences to empower
The Silent Ache: Mastering Daily Life with Bursitis Author: ItHurts.com A Comprehensive Talk on Mastering Daily Life with Bursitis Understanding the Basics: Living with bursitis can feel like a never-ending battle. The sharp twinge of pain in your shoulder as you reach for a cup, the persistent ache in your hip when you stand up, or the throbbing discomfort in your elbow after a long day—these are daily realities for people dealing with this often-overlooked condition. Though bursitis isn’t life-threatening, it significantly impacts quality of life, making it a silent yet relentless ache that requires careful management. Understanding Bursitis: What’s Happening in Your Body? Bursitis occurs when the small, fluid-filled sacs (called bursae) that cushion bones, tendons, and muscles near joints become inflamed. This inflammation leads to pain, stiffness, and swelling. Common sites for bursitis include: – Shoulders: Often due to repetitive overhead movements. – Elbows: A result of pressure or trauma, such as leaning on hard surfaces. – Hips: Frequent in people who run, climb, or have imbalances in posture. – Knees: Known as “housemaid’s knee,” this can be caused by prolonged kneeling. – **Heels or Ankles:** Often seen in active individuals or those with improper footwear. While bursitis is most commonly caused by repetitive motion or overuse, other factors like aging, obesity, and inflammatory conditions like rheumatoid arthritis can increase risk. Common Challenges of Living with Bursitis Mobility Issues Bursitis can restrict movement in affected joints, making it difficult to perform everyday tasks like bending, lifting, or climbing stairs. 2. Chronic Pain Persistent pain can take a toll not just physically but emotionally. Many individuals feel a sense of helplessness when flare-ups occur unpredictably. 3. Fatigue Pain and restricted mobility often lead to fatigue, as even minor tasks require extra energy. 4. Interrupted Sleep Pain during the night, especially in cases of hip or shoulder bursitis, can disrupt sleep patterns, leaving individuals feeling drained and irritable. 5. Social Isolation When simple activities like attending social gatherings or playing with grandchildren become painful, it can lead to withdrawal and a sense of isolation. Strategies for Navigating Daily Life with Bursitis The good news? With the right approach, you can manage bursitis and reclaim your day-to-day life. Here are practical tips and insights. 1. Prioritize Rest—But Don’t Overdo It Rest is essential for reducing inflammation during a flare-up, but extended inactivity can lead to muscle weakness and stiffness. Strike a balance: – Do: Rest the affected area for 1–2 days during intense pain. – Don’t: Prolong rest for weeks; gentle movement aids recovery. 2. Build a Movement-Friendly Routine Low-impact activities help maintain mobility without worsening bursitis. Incorporate exercises that strengthen supporting muscles and improve joint function: – Walking: Keeps joints moving without overloading them. – Swimming or Aquatic Therapy: Water reduces joint strain while promoting mobility. – Stretching: Gentle stretches tailored to the affected area prevent stiffness. 3. Apply the R.I.C.E. Method When bursitis flares up, the R.I.C.E. method (Rest, Ice, Compression, Elevation) is a quick and effective remedy: – Rest: Avoid movements that trigger pain. – Ice: Apply ice packs for 15–20 minutes every few hours. – Compression: Use an elastic bandage to reduce swelling. – Elevation: Keep the affected joint elevated, if possible. 4. Ergonomics Matter Reevaluate your workspace, home environment, and posture to prevent repetitive strain. Consider: – Ergonomic Chairs: Support the back and hips properly. – Adjustable Desks: Reduce shoulder and elbow strain. – Cushioned Mats: Ease knee pressure if standing for long periods. 5. Manage Pain with Care Over-the-counter options like ibuprofen or acetaminophen can reduce pain and inflammation. However, always consult your doctor if: – Pain persists despite medication. – You experience side effects like stomach upset. Natural remedies, such as turmeric or omega-3 supplements, may also help reduce inflammation. 6. Physical Therapy Physical therapists can create tailored plans to improve strength and flexibility in affected joints. Therapies may include: – Ultrasound Therapy: Stimulates healing in deep tissues. – Manual Therapy: Restores joint function. – Targeted Exercises: Focused strengthening for joint stability. 7. Address Underlying Causes If bursitis results from poor posture or repetitive strain, addressing the root cause is crucial. Small changes, like adjusting your walking gait or strengthening your core, can reduce recurrence. Mental Health and Emotional Resilience Living with bursitis isn’t just a physical challenge; it’s an emotional one. Chronic pain can lead to frustration, anxiety, and even depression. Building emotional resilience is key: 1. Talk to Someone Join a support group or online forum where others share their bursitis experiences. Knowing you’re not alone can be comforting. 2. Practice Mindfulness Meditation, yoga, or simple breathing exercises can help reduce stress and make pain more manageable. 3. Celebrate Small Wins Improvement can feel slow, but small progress—like reduced pain after stretches or a good night’s sleep—deserves celebration. When to Seek Medical Intervention If bursitis symptoms persist or worsen, it may require medical intervention. Doctors might recommend: – Corticosteroid Injections: Provide relief by reducing inflammation directly. – Aspiration: Draining excess fluid from the bursa. – Surgery: Rarely needed, but it’s an option for severe, recurring cases. Proactive Prevention: Protect Your Joints While bursitis can be managed, preventing flare-ups is even better. Adopt these habits to keep your joints healthy: – Warm-Up Before Activity: Prepare joints for movement with light stretches. – Avoid Repetitive Motion: Take breaks during activities that strain joints. – Maintain Healthy Weight: Reduces stress on weight-bearing joints. – Wear Proper Footwear: Good support can prevent hip and knee issues. Tools to Make Life Easier Adopting the right tools can significantly ease the strain of daily activities. Here are a few recommendations: – Supportive Pillows: Relieve pressure on shoulders and hips during sleep. – Compression Sleeves: Provide joint support for elbows, knees, or ankles. – Knee Pads or Cushioned Mats: Ideal for those who kneel frequently. Final Thoughts: Endometriosis is more than a physical condition; it’s an emotional a Bursitis may be a silent ache, but it doesn’t have to define your life. By understanding the condition, addressing
Living in the Shadow of Pain: The Impact of Endometriosis on Mental Health and Relationships Author: ItHurts.com A Comprehensive Talk on Living in the Shadow of Pain: Endometriosis Understanding the Basics: Living with endometriosis is often an invisible struggle, yet its impacts can be profoundly visible in the lives of those it touches. Affecting approximately 1 in 10 individuals assigned female at birth, endometriosis is a chronic condition where tissue similar to the lining of the uterus grows outside it, causing debilitating pain, infertility, and a host of other symptoms. But while the physical toll is significant, the emotional and relational burdens of endometriosis are often underestimated. The Mental Health Toll of Endometriosis A Cycle of Chronic Pain and Psychological Distress Living with endometriosis often means enduring relentless physical pain. Chronic pain can lead to increased levels of cortisol, the stress hormone, which in turn can heighten anxiety and lower one’s threshold for handling further stressors. For many, the physical discomfort of endometriosis is matched—or even exceeded—by the emotional weight of living with an unpredictable, often misunderstood condition. Depression and Anxiety Studies have shown that individuals with endometriosis are significantly more likely to experience depression and anxiety. This is no surprise, considering the condition often impacts one’s ability to work, maintain an active social life, and even engage in basic self-care. Pain flare-ups can be isolating, leading to feelings of loneliness and hopelessness. Furthermore, uncertainty about when symptoms might strike next can create an ongoing state of anxiety. Body Image and Self-Esteem Issues Endometriosis often affects self-esteem, particularly for those who experience infertility, bloating, or weight fluctuations as part of their symptoms. The societal pressure to maintain a certain image, combined with the emotional toll of not being able to meet cultural or personal expectations regarding fertility, can exacerbate feelings of inadequacy and low self-worth. The Hidden Grief of Endometriosis Endometriosis often brings with it a sense of loss—loss of health, normalcy, and sometimes the ability to have biological children. This grief can be ongoing, compounded by frustration over medical dismissals or delayed diagnoses, which average seven to ten years. Unprocessed grief can fuel feelings of anger, sadness, and resentment, creating a barrier to mental and emotional healing. How Endometriosis Affects Relationships Romantic Relationships Impact on Intimacy One of the most challenging aspects of endometriosis in romantic relationships is its impact on intimacy. Pain during intercourse (dyspareunia) is a common symptom, leading many individuals to avoid sexual activity altogether. This can strain even the most understanding partnerships, as feelings of rejection or guilt often arise on both sides. The Burden of Caregiving Partners of individuals with endometriosis often take on caregiving roles, which can lead to emotional burnout. They may struggle to balance their empathy for their partner’s pain with their own unmet needs for connection, intimacy, or shared activities. Communication Breakdowns If not addressed openly, endometriosis can lead to misunderstandings and resentment. A lack of education about the condition can cause some partners to underestimate its impact, dismissing symptoms as “just bad cramps.” This invalidation can erode trust and intimacy in the relationship. Platonic Relationships Social Isolation Living with chronic pain often means canceling plans or withdrawing from social activities, which can strain friendships. Over time, some individuals with endometriosis may feel misunderstood or forgotten, leading to further isolation. Emotional Burdens Friends may not always know how to support someone with a chronic illness. They might offer well-meaning but unhelpful advice or unintentionally minimize the condition, causing hurt feelings and a sense of alienation. Workplace Relationships Endometriosis can also affect professional relationships, as frequent absences or the inability to perform at full capacity may lead to misunderstandings with colleagues or employers. This can further impact one’s mental health, creating a vicious cycle. Strategies for Navigating the Emotional and Relational Impacts of Endometriosis Acknowledge the Emotional Toll Recognizing and validating the emotional impact of endometriosis is an essential first step. Therapy can be particularly beneficial in helping individuals process grief, build coping mechanisms, and develop strategies for navigating relationships. Action Tip: Consider seeking a therapist experienced in chronic illness. Cognitive-behavioral therapy (CBT) can be especially effective in addressing anxiety and depression linked to chronic pain. 2. Educate Yourself and Others Education is key to fostering understanding. Whether it’s sharing articles with loved ones or attending informational sessions together, learning about endometriosis can help bridge the gap between those living with the condition and their support networks. Action Tip: Compile a list of reputable resources about endometriosis and share it with your partner, friends, or family. Encourage them to ask questions and engage in conversations about your experience. 3. Foster Open Communication Being open about symptoms, needs, and emotions is vital in maintaining healthy relationships. In romantic partnerships, discussing how endometriosis affects intimacy can help reduce feelings of guilt or rejection. For friendships, honesty about physical and emotional limitations can prevent misunderstandings. Action Tip: Use “I” statements to express feelings without placing blame. For example, “I feel overwhelmed when my pain isn’t acknowledged” instead of “You never take my pain seriously.” 4. Set Boundaries Setting boundaries is an important form of self-care. This might mean declining invitations during flare-ups or explaining limits to what you can contribute in relationships. Healthy boundaries protect emotional energy and prevent resentment. Action Tip: Practice saying, “I can’t do that right now, but I’d love to when I’m feeling better.” This reinforces your willingness to engage while respecting your limitations. 5. Build a Support System Isolation exacerbates the challenges of living with endometriosis. Connecting with others who understand the experience, whether through local support groups or online forums, can provide validation and encouragement. Action Tip: Look for endometriosis-focused support groups on platforms like Facebook or through organizations like the Endometriosis Association. Sharing stories and tips with others in similar situations can be empowering. 6. Explore Alternative Approaches to Intimacy For couples struggling with the sexual impacts of endometriosis, exploring alternative forms of intimacy can be healing. Emotional closeness, non-sexual physical affection, and open discussions about
Through the Darkness: Personal Stories of Pain and Resilience in Depression and Chronic Pain Author: ItHurts.com A Comprehensive Talk on Depression and Chronic Pain Understanding the Basics: Living with depression is a challenge in itself, but when coupled with physical pain, it can feel like an unrelenting battle. For many, this dual burden creates a complex web of emotional and physical struggles that are hard to untangle. Yet, stories of resilience and recovery abound, offering hope and a sense of community to those who feel alone in their journey. In this article, we share deeply personal narratives from individuals living with both depression and physical pain. These stories provide unique insights into coping mechanisms, treatments, and advice for others walking a similar path. Emma’s Story: The Weight of Fibromyalgia and Depression Emma, 36, was diagnosed with fibromyalgia five years ago. The chronic pain and fatigue were debilitating, but the depression that accompanied it made life feel unbearable. > “The pain was one thing, but the feeling of worthlessness that came with not being able to work or even get out of bed some days was crushing. I felt like I was failing everyone around me.” Emma credits her turning point to finding a support group that specialized in both chronic pain and mental health challenges. > “Hearing other people’s stories made me realize I wasn’t alone. One woman shared how journaling helped her identify patterns between her emotional lows and physical flares. I started doing the same and discovered that pacing myself—not just physically but emotionally—helped tremendously.” Today, Emma uses a combination of medication, cognitive behavioral therapy (CBT), and mindfulness practices to manage her symptoms. She also emphasizes the importance of self-compassion. > “On days when I can’t do much, I remind myself it’s okay. Healing isn’t linear.” Sophia’s Battle: Arthritis and Postpartum Depression Sophia, 29, developed severe arthritis after giving birth to her first child. The physical pain made it difficult to care for her newborn, and postpartum depression compounded her struggles. > “I felt like I was failing as a mother. Every diaper change, every feeding, was a reminder of what I couldn’t do as easily as other moms.” Sophia found help through an online community of mothers dealing with chronic illnesses. > “It was such a relief to talk to other women who got it. They shared tips on baby care that didn’t aggravate my pain and reminded me that being a good mom isn’t about being perfect.” In terms of treatment, Sophia combines anti-inflammatory medications with antidepressants and prioritizes rest whenever possible. She also swears by using adaptive parenting tools like ergonomic baby carriers and voice-activated assistants to lighten her load. > “The biggest lesson I’ve learned is to ask for help and accept it. You can’t pour from an empty cup.” Liam’s Journey: Coping with a Back Injury and Depression Liam, 42, was an active runner until a severe back injury sidelined him two years ago. The chronic pain was a constant reminder of what he had lost, and the depression that followed made it hard to find joy in anything. > “I’d stare at my running shoes and feel this deep, aching sadness. Running wasn’t just exercise for me; it was my therapy.” Liam’s breakthrough came when his physical therapist recommended swimming as a low-impact alternative. Initially hesitant, he found solace in the water. > “Swimming became my meditation. It didn’t just help with the pain—it gave me something to look forward to, a new goal.” He also sought help from a therapist who introduced him to Acceptance and Commitment Therapy (ACT). > “ACT taught me that it’s okay to feel pain, both physical and emotional. Fighting it all the time just made things worse. Accepting it didn’t mean giving up; it meant learning to live alongside it.” Liam now advocates for physical activity, even in small doses, as a way to manage both depression and chronic pain. James’ Struggle: Migraines, Depression, and the Road to Recovery For James, 50, migraines were a constant in his life since his late twenties. The intense pain, coupled with the unpredictability of attacks, led to severe depression. > “There were days I just wanted to disappear. How do you plan a life when you never know if you’ll be incapacitated by pain?” James tried countless treatments, from prescription medications to dietary changes, with limited success. His turning point came when he began biofeedback therapy. > “Biofeedback taught me how to recognize and control my body’s stress responses. It didn’t cure my migraines, but it reduced their frequency and intensity. That gave me a sense of control I hadn’t felt in years.” James also found solace in volunteering, which helped him shift his focus outward. > “Helping others gave me a purpose. It reminded me that pain doesn’t have to define me.” Today, James uses a combination of therapies, including biofeedback, meditation, and regular exercise, to manage his symptoms. Lessons from These Stories These personal narratives highlight the complex interplay between physical pain and depression. While each journey is unique, several common themes emerge: – The Importance of Support: Whether it’s a support group, a therapist, or an online community, connecting with others can be a powerful source of healing. – Finding the Right Treatment: There’s no one-size-fits-all solution. It often takes time and experimentation to find the right combination of treatments. – Self-Compassion Matters: Accepting your limitations and treating yourself with kindness is crucial for both physical and emotional recovery. – Purpose Can Heal: Engaging in meaningful activities, whether through work, hobbies, or volunteering, can provide a sense of control and fulfillment. Advice for Readers If you’re struggling with both physical pain and depression, remember these key takeaways: Seek Help Early: Don’t wait to reach out to a healthcare professional. The sooner you address your symptoms, the better your chances of managing them effectively. Build Your Toolbox: Experiment with different treatments and coping mechanisms. What works for someone else may not work for you, and that’s